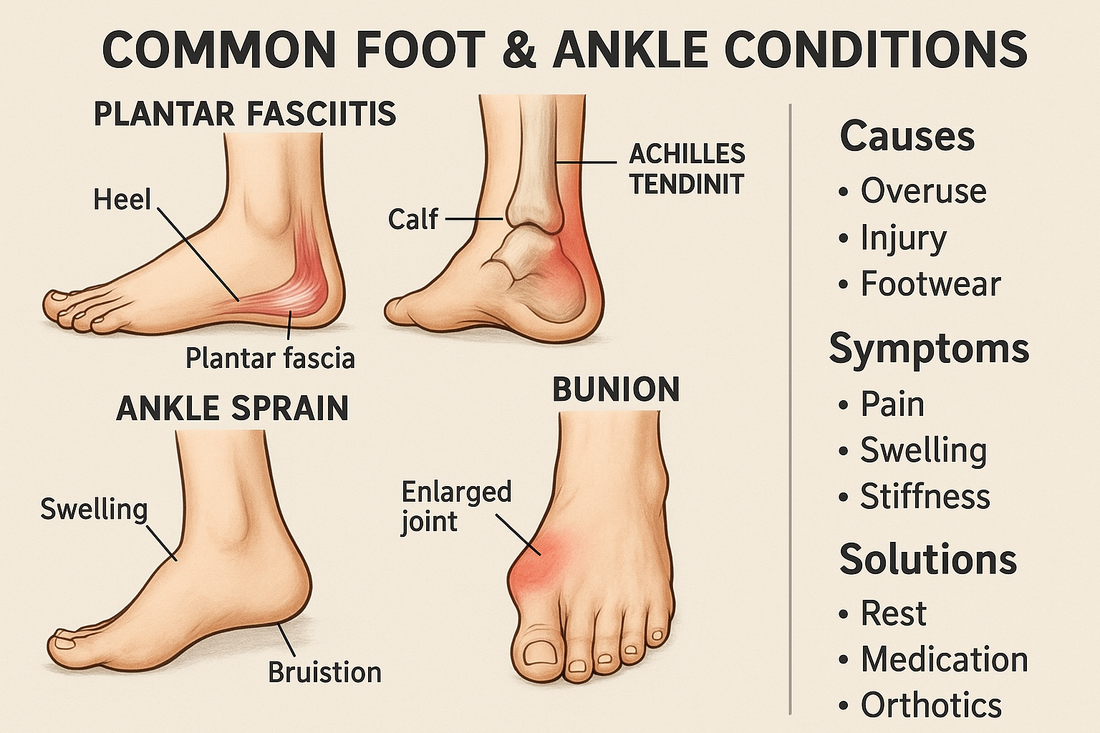
Common Foot & Ankle Conditions: Causes, Symptoms & Solutions
Share
Healthy feet and ankles are critical to mobility, comfort, and overall well-being. Unfortunately, many people suffer from foot or ankle conditions that, if untreated, can worsen over time. Below is a guide to several common problems, along with what causes them, how to recognize them, and what you can do (from self-care to when to see a specialist).
1. Plantar Fasciitis
What it is / cause
Plantar fasciitis is the inflammation or microtearing of the plantar fascia — the thick band of tissue that runs from your heel bone to your toes. It often arises from overuse (running, long standing), poor foot biomechanics (flat feet or high arches), obesity, or wearing unsupportive footwear.
Symptoms
- Sharp, stabbing heel pain, especially first thing in the morning or after rest
- Pain that improves slightly with movement but may worsen later in the day
- Tightness or stiffness in the arch or heel
Solutions / management
- Rest, ice, and NSAIDs (if medically appropriate)
- Stretching exercises, especially calf and Achilles stretches
- Use of orthotics or arch support (e.g. firm insoles or custom inserts)
- Night splints to maintain dorsiflexion
- Cushion gel heel pads to absorb impact
- If pain persists >6–12 months or is severe: see a podiatrist for potential corticosteroid injections or other interventions
2. Achilles Tendinopathy / Tendinitis
What it is / cause
This is inflammation or degeneration of the Achilles tendon (the tendon attaching calf muscles to the heel). It’s often caused by sudden increases in activity, tight calves, poor footwear, or biomechanical issues.
Symptoms
- Pain and stiffness along the back of the heel or lower leg, especially in the morning
- Swelling, thickening, or tenderness along the tendon
- Pain with heel raises or pushing off
Solutions / management
- Eccentric calf strengthening (slow lowering exercises)
- Stretching of calf muscles
- Heel lifts or cushion heel inserts to reduce strain
- Avoid sudden increases in activity; cross-train with low impact
- Use supportive shoes with good heel counter
- Physical therapy modalities (e.g. ultrasound, shockwave)
- In persistent cases: surgical options
3. Bursitis (e.g. Retrocalcaneal Bursitis)
What it is / cause
Inflammation of a bursa (fluid-filled sac) near joints or tendon attachments. In the heel, a common type is retrocalcaneal bursitis, which lies between the Achilles tendon and heel bone. Causes include repetitive pressure, overuse, tight shoes, or biomechanical stress.
Symptoms
- Localized swelling, warmth, and tenderness just in front of or below the Achilles insertion
- Pain when compressing the area or during dorsiflexion
- Redness or increased rubbing if shoes irritate the area
Solutions / management
- Reduce irritation - wear shoes with a softer heel counter or open-back designs
- Use heel cushion pads or gel sleeves to offload pressure
- Ice, rest, NSAIDs
- Gentle stretching and range-of-motion exercises
- If chronic or very painful: medical evaluation and possibly corticosteroid injection
4. Ankle Sprain / Ligament Injury
What it is / cause
A sprain is a stretching or tearing of the ligaments around the ankle, usually the lateral (outside) ligaments, due to twisting injuries (rolling the ankle). It’s one of the most common injuries in sports and daily life.
Symptoms
- Sudden pain at the time of injury
- Swelling, bruising, tenderness over ligament(s)
- Difficulty bearing weight or walking
- Instability or “giving way” feeling
Solutions / management
- Immediately apply RICE: Rest, Ice, Compression, Elevation
- Use an ankle brace or support during healing
- Gradual rehabilitation: range-of-motion, strengthening, proprioception (balance) exercises
- Return-to-activity gradually; avoid forcing full activity too soon
- In severe cases: imaging (MRI) and possible surgical repair
5. Bunions (Hallux Valgus)
What it is / cause
A bunion is a bony bump at the base of the big toe, caused by misalignment of the first metatarsal and shifting of the big toe (valgus). It can be aggravated by tight or narrow shoes, genetic predisposition, or foot mechanics.
Symptoms
- Visible bump on the side of the big toe joint
- Redness, swelling, pain or irritation over the bunion
- Difficulty fitting shoes
- Calluses or corns adjacent to the bunion
Solutions / management
- Wear wide, supportive shoes with roomy toe box
- Use toe spacers, bunion pads, or silicone gel sleeves
- Orthotic devices to improve foot alignment
- Night splints or bunion braces
- In severe or painful cases: surgical correction (bunionectomy)
6. Morton's Neuroma
What it is / cause
A thickening of the tissue around a nerve between the toes (most commonly between the 3rd and 4th toes). It can be triggered by repetitive pressure, tight shoes, high heels, or biomechanical stress.
Symptoms
- Burning or sharp pain between the toes or in the ball of the foot
- Sensation of a pebble inside the shoe
- Numbness or tingling in the toes
Solutions / management
- Shoes with wide toe box, low heels
- Metatarsal pads or gel cushions to redistribute pressure
- Avoiding high-impact activity or excessive forefoot load
- Injection therapy (steroid or alcohol) in persistent cases
- Surgical removal of the neuroma (in severe, refractory cases)
7. Posterior Tibial Tendinopathy / Flatfoot
What it is / cause
The posterior tibial tendon supports the arch of the foot. When it becomes inflamed or degenerative, the arch can collapse, creating adult acquired flatfoot. Causes include overuse, obesity, hypertension, and arthritis.
Symptoms
- Pain along the inside of the ankle/foot
- Flattening of the arch, foot turning outward
- Difficulty standing on tiptoe
- Swelling along the tendon
Solutions / management
- Orthotics or ankle-foot orthoses (AFO) to support arch
- Strengthening and foot posture correction exercises
- Immobilization or bracing in more advanced cases
- Surgical correction (tendon repair, osteotomies) if structural deformity exists
General Preventive Tips & Self-Care Strategies
- Choose supportive, well-fitting footwear with cushioning and proper arch support
- Avoid sudden increases in activity; increment training gradually
- Incorporate stretching (especially calves, Achilles, plantar fascia) into regular routine
- Maintain a healthy weight to reduce load on feet
- Use gel pads, cushions, or orthoses when needed
- Alternate surfaces and shoes to reduce repetitive stress
- Monitor foot health, especially if you have diabetes, vascular disease, or neuropathy
- Seek early evaluation if pain persists beyond 1–2 weeks or is severe
When to Consult a Specialist
You should see a podiatrist, orthopedic foot & ankle surgeon, or physical therapist if:
- Pain is severe, worsening, or limiting daily function
- Symptoms persist beyond several weeks of home care
- You experience numbness, tingling, or loss of sensation
- There’s deformity, instability, or structural changes
- You have underlying conditions (e.g. diabetes, peripheral vascular disease)
How 26 Apothecary Can Help
At 26 Apothecary, our mission is to support foot and ankle wellness through non-surgical solutions and high-quality podiatric products. 26Apothecary
Here are ways you can incorporate them into managing or preventing common conditions:
- Orthotic Inserts & Sports Orthotics: Provide arch support and redistribute pressure
- Cushion Gels & Gel Pads: Enhance shock absorption and reduce localized pressure
- Heel Gel Cushions: Help with plantar fasciitis or heel pain
- Supports, Splints & Braces: Stabilize joints, reduce strain on tendons/ligaments
- Compression & Tape Products: Assist swelling control and proprioception
By combining appropriate self-care, early intervention, and supportive products, many foot and ankle conditions can be managed effectively without invasive surgery.
